Integrated Care for Dual Eligible Beneficiaries
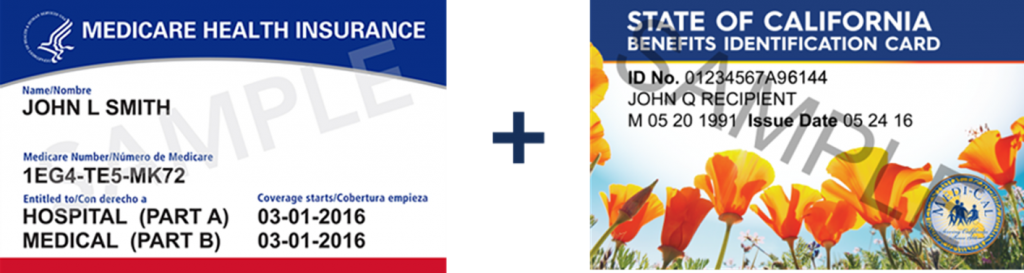
Dually eligible beneficiaries are people enrolled in both Medicare and Medi-Cal. Medicare is the primary payer for acute and post-acute care services. Medi-Cal wraps around Medicare by providing assistance with Medicare premiums and cost sharing, and by covering some services that Medicare does not cover, such as long-term services and supports (LTSS). As part of CalAIM, DHCS is implementing policies to promote integrated care for beneficiaries dually eligible for Medicare and Medi-Cal.
Enrollment Information
The Future of Cal MediConnect
On January 1, 2023, Cal MediConnect plans will transition to Medicare Medi-Cal Plans (MMPs or Medi-Medi Plans) provided by the same plans as Cal MediConnect. Cal MediConnect members will be seamlessly transitioned by their health plans. Learn More
Medicare Advantage Information for Dual Eligible Beneficiaries
Like all Medicare beneficiaries, dual eligible beneficiaries can choose whether to receive care through Original Medicare, or enroll in a Medicare Advantage (MA) plan, sometimes called “Part C” or “MA Plans.” Some Medicare Advantage options for dual eligibles in California changed effective January 1, 2023. Learn More
Medi-Cal “Matching Plan Policy” for Dual Eligible Beneficiaries
To address the challenges of coordinating across different health plans for Medicare and Medi-Cal benefits, DHCS has a Medi-Cal matching plan policy in 12 counties. Under this policy, a beneficiary’s Medicare plan choice is the lead, and the Medi-Cal plan follows. Learn More
Statewide Medi-Cal Managed Care Enrollment for Dual Eligible Beneficiaries
Most dually eligible beneficiaries not already enrolled in Medi-Cal managed care will be newly enrolled in Medi-Cal plans in 2023. Medi-Cal Plans provide wraparound services and care coordination dual eligible beneficiaries, particularly for Long-Term Services and Supports.
Duals Alignment Statewide Directory
For information by county on current and future Medi-Cal enrollment options, please see this list. Learn More
Resources for Complaint Resolution for Beneficiaries with Medicare and Medi-Cal
In California there are a variety of Ombudsperson programs ready to assist beneficiaries. The primary duties of an Ombudsperson program is to help individuals explore and assist them in determining options to help resolve conflicts and to bring systemic concerns to the attention of those best suited to solve the problem.Learn More
Policy Resources
Medicare Advantage Information for Dual Eligible Beneficiaries
Like all Medicare beneficiaries, dual eligible beneficiaries can choose whether to receive care through Original Medicare, or enroll in a Medicare Advantage (MA) plan, sometimes called “Part C” or “MA Plans.” Some Medicare Advantage options for dual eligibles in California changed effective January 1, 2023. Learn More
Duals Eligible Special Needs Plans in California
Dual Eligible Special Needs Plans (D-SNPs) are Medicare Advantage (MA) health plans which provide specialized care and coordination for dual eligible beneficiaries. Learn More
Duals Special Needs Plans Contract and Policy Guide
All D-SNPs in California must have executed contracts with the Department of Health Care Services (DHCS), the state Medicaid agency. DHCS also maintains a D-SNP Policy Guide, with further requirements for D-SNPs. Learn More
Dual Special Needs Plans Quality and Data Reporting
D-SNPs have robust reporting requirements for both Medicare and Medi-Cal.DHCS monitors D-SNPs for the quality of care and health equity provided to members in Medi-Cal through state-specific reporting requirements. Learn More
Statewide Managed Long-Term Care
CalAIM is transitioning institutional long-term care to managed care statewide to better coordinate care, simplify administration, and provide a more integrated experience. Learn More
Alzheimer’s Disease and Related Dementias
DHCS is utilizing the Dementia Care Aware initiative to establish a statewide standard for diagnosing Alzheimer’s Disease and Related Dementias. Learn More
Workgroups
CalAIM Managed Long-Term Services & Supports & Dual Integration Workgroup
The CalAIM MLTSS and Duals Integration Workgroup is a stakeholder collaboration hub, including health plans, providers, advocates, other stakeholders, and the U.S. Centers for Medicare & Medicaid Services (CMS).
Quarterly Coordinated Care Initiative Stakeholder Webinar
Building upon many years of stakeholder discussions, the Coordinated Care Initiative established Cal MediConnect and fostered many local collaborations to support integrated care for dual eligible beneficiaries. This webinar series provides updates on quality measures, best practices, and emerging issues.
Questions and Comments
Contact DHCS with any questions or comments about Integrated Care for Dual Eligible Beneficiaries at info@calduals.org.